The following article is written by Marketing and Communications Coordinator, Cristina Threlkeld for the National Infusion Center Association.
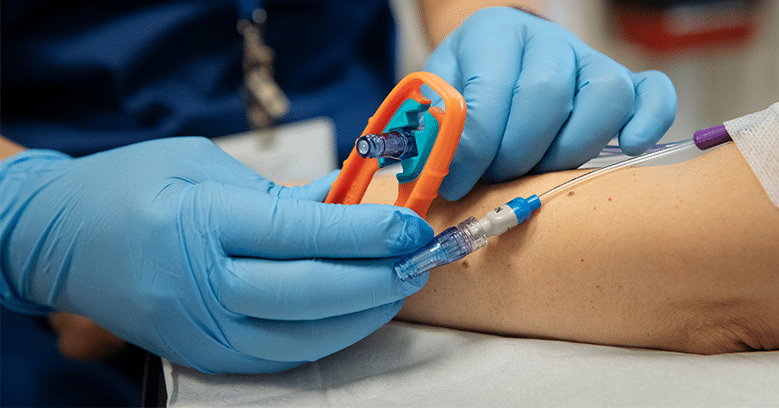
Patients rely on easy and affordable access to their medications. Prescribing clinicians and sites of treatment also rely on accessibility and the flexibility to obtain these medications in the most cost-effective and seamless way possible.
In 2020, BlueCross BlueShield of Tennessee (BCBST) enacted a specialty pharmacy mandate (i.e., mandatory white-bagging) requiring that the doctors of some of the nation’s most vulnerable patients obtain their medications through a specialty pharmacy. What appears to be an isolated shift could indicate a trend among insurance companies, which spells trouble for patients and providers across the nation.
A patient’s health is completely dependent upon their ability to receive the right medication at the right time – and in an affordable and accessible setting. Typically, infusion centers operate on a buy-and-bill model. Under such a model, the site of care—for example, an office-based infusion center—buys and maintains an inventory of medications. They administer the prescribed medication in the correct amount to their patients and then bill the insurer after treatment. This model enables the infusion center to buy and store the appropriate amount of medications and from their preferred sources.
A specialty pharmacy mandate, such as the one proposed by BCBST, takes away providers’ flexibility in managing their business and affects how they care for patients. It even raises questions of ethics: Should insurance companies get in between providers and their patients by stipulating how providers acquire their medications and care for their patients? Is it ethical to require acquisition of drug through a specialty pharmacy when insurers own specialty pharmacies?
NICA has seen similar trends in benefit and policy changes in various states, most recently in Delaware and Pennsylvania, in addition to Tennessee. These all appear to be cost-driven strategies intended to minimize insurers’ costs, increase rebate revenue, and reduce utilization of cost-share assistance programs.
The result of a specialty pharmacy mandate would ultimately affect the health of the patient. As many clinicians know, there is serious risk and lots of time involved with coordinating care for infusion patients, and it must be done in order to ensure that patients are receiving high-quality medication preparations in a safe environment. Infusion centers will not be able to sustain with the lost revenue, and the result could mean that these sites of care would be forced to send patients to a more expensive location – likely a hospital-setting. As many patients already struggle with affordability of care within the most cost-effective care settings, most will not be able to afford their care if this happens.
The sustainability of sites of cares’ business models would also be jeopardized. Providers will struggle to keep providing the same inexpensive care at the high level of service that makes the experience so great for them. Clinicians pride themselves on being able to administer these life-changing medications more affordably and in a more comfortable setting than hospitals, and patients rely on this service to benefit their healing journeys. The shorter wait times, the personalized service, and the ability to receive treatment in the most affordable manor are all crucial to the patient’s ability to continue necessary care, to feel cared for and ultimately contribute to their healing. A specialty pharmacy mandate would ruin the chances of treatment centers being able to continue to care for patients in the way that they do.
What seems like one isolated, ill-informed decision on behalf of BlueCross BlueShield of Tennessee could signal a future filled with turmoil, restricted access, and poorer health outcomes. Despite the uncertainty, one thing remains clear: healthcare providers are committed to improving the lives of others. Providers need the flexibility and autonomy to provide the best care to their patients at the lowest cost. Introducing middlemen into that equation generally impedes the care continuum.
If you are a provider in Tennessee and would like to voice your opinion on specialty pharmacy mandate, please use our grassroots platform to do so at http://bit.ly/BCBSTNProvider. You can encourage your patients to get involved at http://bit.ly/BCBSTNPatients.
Please keep an eye on our social media for the announcement of our Advocacy Toolkit! The toolkit will house template letters and information for current initiatives, such as this BlueCross BlueShield of Tennessee specialty pharmacy mandate issue.