AUSTIN, Texas (September 9, 2025) — The overwhelming majority of small and independent healthcare providers fear that Medicare’s upcoming negotiation of Part B drug prices could inadvertently curb patients’ access to certain lifesaving medicines, according to results from a survey conducted by Avalere Health and released in partnership with the National Infusion Center Association (NICA).
“Community infusion centers are often the only access point for patients needing complex therapies, particularly in underserved areas,” said Brian Nyquist, MPH, president and CEO of NICA. “This survey highlights providers’ concerns that well-intended price negotiations could unintentionally reduce their ability to offer these treatments. When providers can’t sustain access, its patients who pay the price. Policymakers have an opportunity to work with us to ensure cost-saving efforts strengthen — not weaken — the care infrastructure patients depend on.”
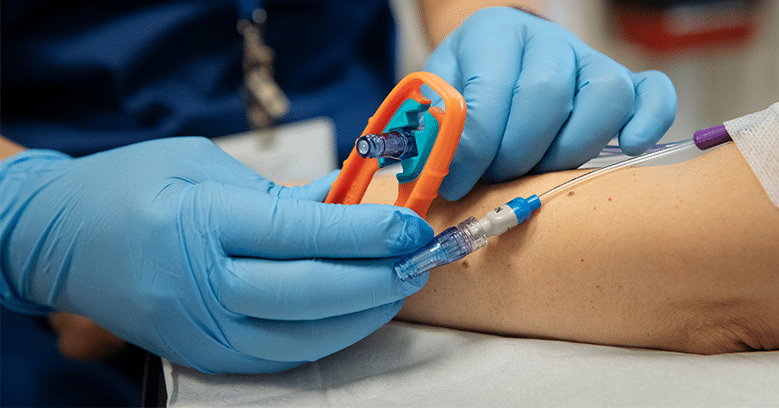
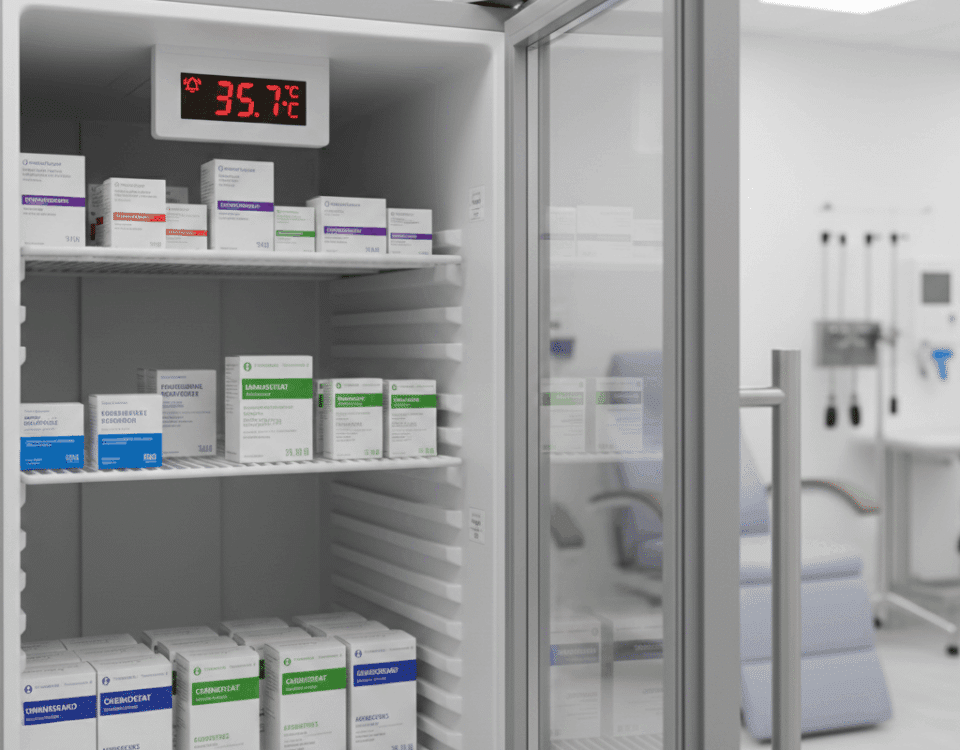
Medicare reimbursements for provider-administered intravenous and injectable medicines are expected to plummet in 2028 when the negotiated prices for the first Part B drugs likely to be negotiated take effect. Reimbursement for Part B drugs is currently calculated as the average sales price of the drug, plus a 6% add-on. But under the Inflation Reduction Act, Medicare will instead use the much lower negotiated Maximum Fair Price (MFP) in place of the average sales price, effectively shrinking the add-on payments that providers receive by up to 50%.[1]
The survey found that 92% of providers report being somewhat or very likely to stop stocking negotiated drugs. Roughly eight in 10 expect price negotiations to impact patient access to medications, and approximately seven in 10 anticipate negative patient health outcomes. Further, nearly three-quarters of providers anticipate operational disruptions, and almost all agree that reimbursement cuts would compromise physician-patient decision-making.
“Everyone shares the goal of making medicines more affordable, but it is critical that affordability not come at the cost of access,” Nyquist said. “This survey makes clear that without thoughtful implementation, Medicare’s negotiation policy could unintentionally restrict patient options and disrupt continuity of care. By engaging providers early and often, policymakers can craft solutions that both manage costs and safeguard patients’ ability to receive the right therapy, at the right time, in a cost-effective setting.”
The survey, conducted by Avalere Health between May 14 and May 29, 2025, received responses from 304 non-hospital healthcare providers across 41 states, including physicians, nurses, and practice administrators.
Click here to review the full set of survey results.
About the National Infusion Center Association: NICA is an independent, nonprofit trade association and accrediting body dedicated to representing ambulatory outpatient care settings where provider-administered biologics and specialty medications are prepared and administered. The NICA Standards of Excellence for Ambulatory Infusion Centers are intended to pertain to all ambulatory care settings where patients receive non-hazardous provider-administered medications via parenteral (i.e., intravenous, intramuscular, subcutaneous, or intradermal) routes.
For more information about NICA, please visit https://infusioncenter.org/.
[1] Avalere Health. Commercial Spillover Impact of Part B Negotiations on Physicians. Available here.