By: Pamela McIntyre, CRNI, IgCN, OCN, and VA-BC
Maximizing Efficiency in Ambulatory Infusion Centers
When it comes to maximizing efficiency in ambulatory infusion centers, one of the most frequently asked questions infusion center managers have is how to determine the appropriate ratio of nurses to patients at their infusion centers. This is a valid concern as we all grapple with maintaining fiscal viability in the era of reimbursement challenges and retention of skilled team members. The key to achieving a suitable staffing model is to balance efficiency with patient safety. This is easier said than done, with several aspects factoring into the equation. Considering the original implementation of outpatient infusion care and early infusions of biologic medications occurred in the oncology space, there is much knowledge to be gained from observing operational efficiencies in this realm. Many opinion papers are available that have analyzed oncology infusion operations, and the consensus is that the acuity of patients drives the nurse-to-patient ratio. This data can be extrapolated to other ambulatory infusion clinic settings with similarities in monitored infusions, and evaluating time-driven components specific to the acuity of the drugs being administered is but one of the variables that factors into effective operations.
The ‘National Comprehensive Cancer Network (NCCN) Infusion Efficiency Workgroup Study: Optimizing patient Flow in Infusion Centers’ focused on wait times, calculated at an alarming 25-102 minutes for each patient. This finding supports optimizing patient workflow in the ambulatory infusion center to maintain schedule integrity and minimize overtime costs. Considering that patients frequently struggle to fit their infusion appointments into their daily lives, extended time in the waiting room signals organizational inefficiency, which must be addressed promptly to ensure your reputation in the community and maintain a competitive edge. Patients deserve a consistent timeline so they can depend on the time allotted for their treatments, and adhering to the scheduled appointment time allows our clients to schedule their day reliably, attaining a key goal of outpatient care.
Moving Patients through the System: The Ambulatory Infusion Center Setting
How, then, do we move patients through the system expedited while providing personalized care with patient safety as a focus and moving patients through the queue as quickly as possible?
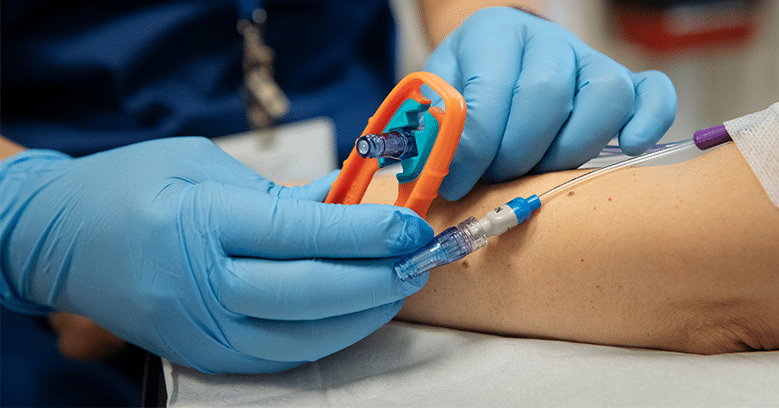
For the non-oncology ambulatory infusion center setting, it is important to distinguish between medications that do not require titration or monitoring throughout the infusion and biologic therapies that require scheduled monitoring and rate titration. Reason would imply that adequate staffing leads to more efficient appointments, particularly concerning biologic and Ig infusions. Escalations in rate are dependent on careful observation for early signs of reaction to a medication, which is accomplished more reliably by having adequate staff in the center to monitor these infusions. Medical assistants can be a valuable method of stretching nurses’ availability, but vital signs are only one of the components of an assessment. Evaluation of those vital signs, as well as any other symptoms, must be documented by a licensed nurse with each vital sign measurement. Nursing staff with the bandwidth to make timely appraisals of their patient’s condition can escalate the infusion rate reliably, maximizing your center’s efficiency and making infusion chairs available on schedule.
Balancing Efficiency with Safe Staffing Levels
How do we balance efficiency with safe staffing levels? One key component of organizational efficiency is a scheduling model that accounts for enhanced nursing attention for patients receiving medications that require monitoring. Another variable in the infusion queue is whether a patient needs a peripheral IV started for their infusion, which should be extended in the case of difficult starts. Finally, adequate time to train is a critical time allotment for nurses. Considering that a common complaint from trainees is inadequate time with their preceptor, providing room in the schedule for this valuable interaction will enrich your team and lay the foundation for excellence in patient care.
Mixing medications is a duty performed by nurses in many infusion centers. Lack of allotted time in the schedule to perform this task can lead to the temptation to prepare products before a patient arrives in an effort to streamline workflow. Not only is it advisable to hold mixing the drug until the patient arrives, but I recommend delaying the reconstitution of any product until infusion access has been established. The above-mentioned NCCN study reported that 19% of centers routinely mixed chemotherapy drugs before a patient arrived at the clinic based on predetermined criteria. The JCO Oncology Practice article ‘Improving Outpatient Infusion Clinic Wait Times at a Comprehensive Cancer Center’ (University of New Mexico Comprehensive Cancer Center – UNMCCC) reported that due to their patients’ travel constraints and wasted product, mixing the medication prior to the infusion appointment was not a viable solution considering between 1% and 2.3% of product was wasted, confirming this is not a viable option for high- cost medications. Any projected gains created by mixing products ahead of the patient’s arrival or prior to the IV site being secured can be neutralized with a single loss of medication from an unexpectedly canceled appointment. Even a phone screen cannot assure that a patient will be treated at their scheduled appointment as they may have unforeseen transportation delays or an emergency while en route, requiring them to reschedule and the reconstituted product to be discarded.
We can conclude that there is no hard and fast rule for ambulatory infusion center staffing ratios at this time. Still, businesses can maximize their staffing ratios by accounting for the myriad of variables that affect a clinic’s timeliness. Each organization must evaluate the time nurses spend on tasks other than the actual administration of medication, impacting schedule reliability to a significant degree. The many variables in our service models and therapies are key to an efficient and sustainable staffing plan.
About the Author
With nearly four decades of comprehensive nursing experience, Pamela McIntyre, CRNI, IgCN, OCN, and VA-BC, is considered a subject matter expert in infusion therapy and a transformational leader of nursing programs. Her trademark method of engagement between colleagues has advanced patient care standards and streamlined the specialty of infusion therapy for interdisciplinary teams. Experienced in hospital, clinic, and home infusion sites of care, she provides consulting services to healthcare organizations for infusion program development, staff mentoring, and offers legal review services through her LLC, Expert Infusion Nurse Consulting, with the goal of ‘Advancing Excellence in Infusion’. Pamela has earned a Master’s degree in Nursing Administration and Leadership from Capella University, holds CRNI, IgCN, OCN, and VA-BC certifications, and embraces the mindset of a lifelong learner. Visit www.expertinfusionnurse.com or contact [email protected] for more information.
About the National Infusion Center Association
NICA is dedicated to ensuring that the nation’s infusion centers remain a safe, more efficient, and more cost-effective alternative to hospital settings for consistent, high-quality care.
Infusion providers have a vested interest in the sustainability of the infusion delivery channel and its ability to serve vulnerable patient populations. NICA Provider Members have a voice and a seat at the table to inform NICA’s activities and the opportunity to remain highly engaged in the expansion and optimization of the infusion industry. Learn more about becoming a NICA member here: https://infusioncenter.org/member-partner-page
Is your organization interested in becoming a featured subject matter expert on The Infusion Blog? Email [email protected] to inquire about opportunities for participation.