By: Monica Parsons, RN, BSN
Director, Clinical Education, National Infusion Center Association
Nurturing Excellence: Designing Effective Training and Competency Programs for Ambulatory Infusion Centers
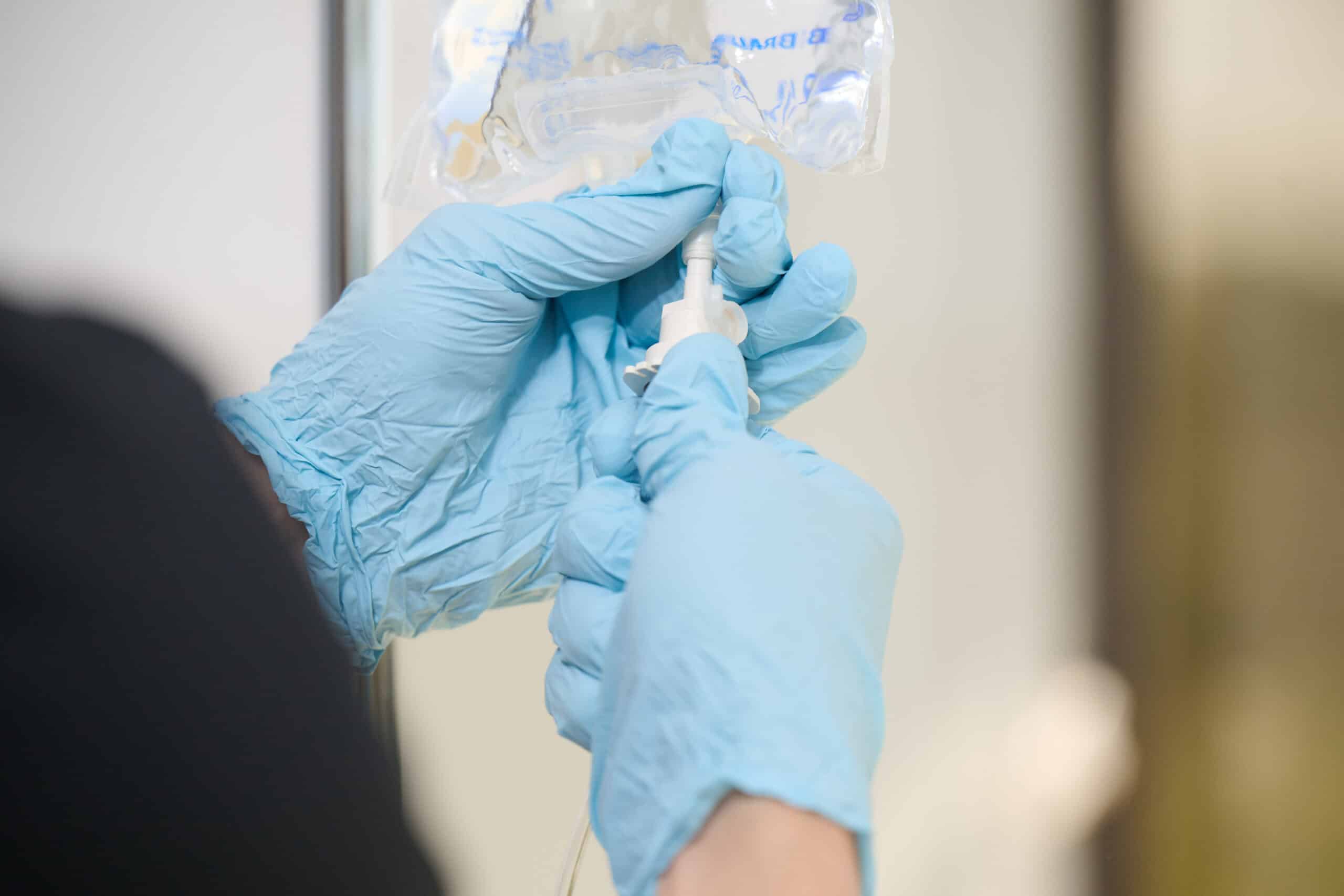
Infusion providers focused on providing excellent patient care often ask themselves, “How do I design a clinical training program that focuses on clinician competency and excellent patient care?” Ambulatory infusion centers cater to a diverse range of patients with varying medical needs. Given the specialized nature of the care provided, investing in a comprehensive training program is imperative for ensuring both personnel and patient safety, optimizing patient and organizational outcomes, and maintaining regulatory compliance. From administering high-risk biologic therapies to managing infusion reactions, the responsibilities and autonomy of those working in infusion centers are multifaceted and require a comprehensive skill set.
The NICA Standards of Excellence for Ambulatory Infusion Centers were developed by infusion experts to serve as a resource for infusion therapy providers to reduce disparities in care quality among office-based infusion settings. NICA Standards support infusion providers’ efforts to implement best practices and provide the basis to ensure providers preparing and administering parenteral medications do so in a safe, consistent, and effective manner. NICA Standards require all organizations to have policies and procedures that detail the education and training program requirements for all personnel. The question remains: how do we develop a training program?
An effective training program begins with a standardized training process. This process should include:
- • Utilizing learning modules and tools to assess comprehension and competency. Consider tailoring all training modules to the learner’s needs.
- • Incorporating multiple methods. Make training as interactive as possible by including pictures, videos, and simulations.
- • Include checkpoints to test the learner’s knowledge and comprehension throughout the learning module.
After education and training are complete, a competency assessment must be completed. Competency assessment tools provide an objective and measurable way to evaluate learning outcomes. Competency assessments may include:
- • written exams,
- • observed clinical competencies and
- • proficiency demonstrations.
Establishing clear competency criteria and conducting regular competency evaluations help identify areas for improvement and ensure ongoing proficiency among staff.
NICA Standards require competency assessment tools be:
- • objective with measurable criteria,
- • contain competency statements with specific performance criteria,
- • identify the method of assessing competence (e.g., demonstration, observation, verbalization),
- • include criteria for achieving success and
- • include the supervisor or validating assessor’s signature.
Competency assessments may include self-assessments, written and/or oral tests, and supervised demonstrations in a simulation setting.
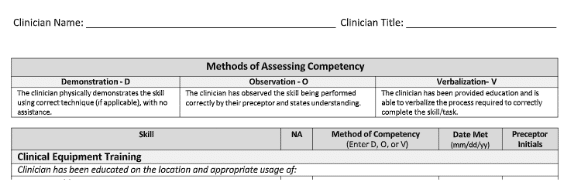
Image: Highlights of various acceptable methods to assess clinical competence.
Ongoing Education and Training
Ensuring that personnel are equipped with the knowledge and skills necessary to excel is an ongoing process. Education programs should consist of three main frequency requirements:
- • initial training upon hire,
- • training at established intervals, and
- • as-needed refresher courses.
A robust education program should provide ongoing education and training at established intervals (most commonly conducted annually) to keep personnel updated on best practices and new therapies. Regular training not only reinforces previous learning but also allows the opportunity to identify and correct deficiencies in the standard of care.
Additional education and training are always provided as a need is identified. As-needed training provides the opportunity to address any gaps in knowledge or skills and correct habits that develop outside of industry standards and best practices.
Patients rely on the delivery of safe, high-quality care. Comprehensive training programs will cultivate a team that is equipped to meet the complex needs of patients while upholding the highest standards of excellence in healthcare delivery. Through continuous education, assessment, and professional development, these centers can remain at the forefront of innovation, ensuring optimal outcomes for patients and advancing the standard of care in ambulatory infusion therapy.
If you have any questions about developing or designing effective training and competency programs for ambulatory infusion centers, you can contact the National Infusion Center Association at [email protected].
About the Author
As the Director of Clinical Education for the National Infusion Center Association, Ms. Parson’s experience as an infusion therapy nurse, Clinical Resource Manager for an MSO, and Director of Quality and Compliance is crucial in her efforts to develop resources and training material to support infusion centers and stakeholders. Prior to joining NICA, Monica successfully led multiple ambulatory infusion clinics through accreditation programs.
About the National Infusion Center Association
NICA is dedicated to ensuring that the nation’s infusion centers remain a safe, more efficient, and more cost-effective alternative to hospital settings for consistent, high-quality care.
Infusion providers have a vested interest in the sustainability of the infusion delivery channel and its ability to serve vulnerable patient populations. NICA Provider Members have a voice and a seat at the table to inform NICA’s activities and the opportunity to remain highly engaged in the expansion and optimization of the infusion industry. Learn more about becoming a NICA member here: https://infusioncenter.org/member-partner-page
Is your organization interested in becoming a featured subject matter expert on The Infusion Blog? Email [email protected] to inquire about opportunities for participation.