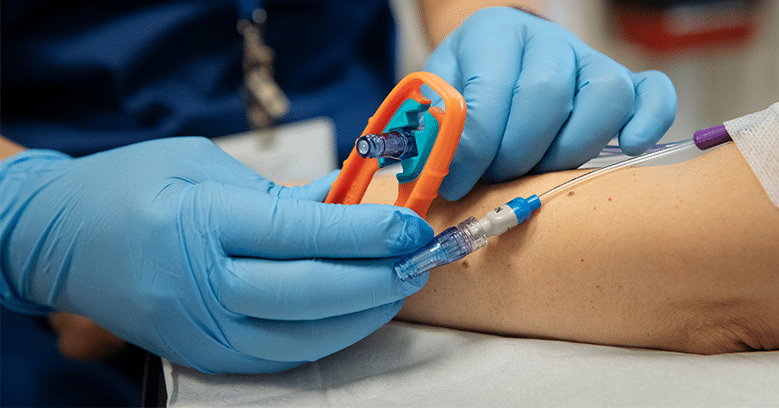
We’ve all been there. You’re chairside with a patient who wants something you know isn’t in their best interest. They ask you to use their “good vein” which happens to be in a risky location. Or they want the infusion rate increased because they’re in a hurry. Sometimes it’s a misunderstanding. Sometimes it’s a deeply held belief or fear. And often, it puts us in a bind. They’re not being difficult — they’re advocating for themselves. But in that moment, it can feel like you’re caught in the crossfire between patient autonomy and professional nursing judgment.
We’re trained to listen, to support, and to advocate — but also to recognize when a clinical boundary needs to be held. Sometimes that means having the difficult conversation, the one where we have to say, “I understand where you’re coming from — but here’s why I’m recommending we approach it differently.”
That tension was the focus of a recent episode of the INS Infusion Room podcast that I had the pleasure of joining, alongside Alicia Barron, Executive Director of the Infusion Access Foundation (IAF), and host Derek Fox, Nurse Educator with the Infusion Nurses Society (INS).
It was an honest, layered conversation about what it feels like to navigate that space — emotionally, ethically, and professionally. We explored how to uphold clinical standards while honoring the patient voice, and the pressures nurses face when making these calls in real time, often without a second to think.
Rethinking “Difficult” Requests
One moment from our conversation has stayed with me since recording. Alicia reframed these situations through the lens of patient autonomy — what it really means, and how often patients feel unheard or disempowered in the healthcare system.
Her insight hit home:
“When patients advocate strongly for themselves, it’s often because they’ve had a history of feeling like no one else has.”
That perspective changes everything. If I can make a patient feel heard and involved in their care—instead of like decisions are being taken away from them—we can shift the dynamic from “me vs. you” to “us vs. the problem.” That shift isn’t just about avoiding conflict. It’s the foundation for building trust, finding common ground, and ultimately getting the best possible care outcomes.
Back-Pocket Phrases for High-Pressure Moments
I recognize that this is hardly the first time you’ve been told to make patients feel heard and involved in their care, but knowing this in theory is one thing—being able to apply it effectively in the heat of the moment is another. You don’t get to pause the conversation, collect your thoughts, and come back with the perfect words. That’s why I’ve learned both as a nurse and as a parent (shout out to Dr. Becky!) to keep a few ready-made phrases in my back pocket. Without them, my brain’s “control room” starts to look like the headquarters in the movie Inside Out during a crisis — alarms blaring, lights flashing, and all the emotions frantically mashing buttons at once. When I have the words ready, I can keep my head clear enough to listen, get curious, and bring the patient into the decision-making process, instead of slipping into a defensive stance.
These aren’t intended to be word-for-word scripts, but rather starting points to keep the patient involved and the tone collaborative.
Invite Their Perspective
Start by opening the door for the patient to share their reasoning, priorities, or concerns. This not only gives you important information to work with, but it also shows the patient that you’re genuinely interested in their point of view. It’s the first step in making the conversation feel collaborative rather than adversarial.
“Tell me more about what’s making you want to do it that way.”
“What is your main concern?”
Validate Their Feelings or Experience
Once you understand their perspective, acknowledge it without immediately trying to change it. Validation doesn’t mean you agree—it means you recognize their feelings or experience as real and important. This helps reduce defensiveness and builds the trust you’ll need for the rest of the conversation.
“I can see why you’d want [request]; [echo their perspective].
“It makes sense that you’d feel frustrated; [echo their perspective]. ”
“I understand why you’d want __________.”
Pivot
After listening and validating, gently shift the conversation toward your professional perspective. The pivot signals that you’ve heard them and are now sharing what you need to consider as their nurse, whether that’s safety, best practice, or clinical guidelines. It’s the bridge between their concerns and your reasoning.
“Here’s what I’m concerned about if we do it that way…”
“Here’s what’s important for me to keep in mind as your nurse…”
“Here’s how I’m looking at this from a safety standpoint…”
Offer Reasoning Without Judgement
It’s important to explain the “why” behind your recommendation in a way that centers safety, evidence, and the patient’s best interest—not blame, criticism, or your own comfort level. The goal is to help the patient understand the risks, benefits, or rationale behind your decision so they feel informed rather than corrected or dismissed. This isn’t about winning an argument—it’s about giving them the context they need to see your recommendation as part of a shared goal. When patients understand why you’re suggesting a certain course of action, they’re more likely to trust the plan, follow through, and stay engaged in their care.
“…the veins in that part of your wrist are smaller and very close to nerves that control movement and feeling in your hand. If one of those nerves gets irritated, it could cause pain or even long-term problems using your hand.”
Enforce the Boundary
Clearly outline what will or won’t happen. There’s no magic phrase that makes someone instantly agree with you—but the words you choose can make a big difference between preserving trust and creating tension. While there’s no one perfect way to say it, there are a few phrases that tend to land the wrong way and can leave the patient feeling shut down, unheard, or like the decision is arbitrary, even when your intentions are good.
“I can’t start the IV there—it’s a site national safety standards tell us to avoid to protect the nerves in your hand. We’ll use this larger vein instead to keep the risk of complications as low as possible.”
Avoid phrases that:
- make it about your personal comfort zone (“I’ve never done it that way”)
- sound rigid or dismissive (“That’s just how we do it here,” “We always do it this way”),
- shift responsibility away from you (“The doctor didn’t order that,” “It’s our policy”).
Instead, link the boundary back to the patient’s safety, best practice, or an evidence-based standard so it’s clear you’re protecting their well-being, not simply enforcing a rule. State it clearly, with a calm tone, then pause—giving them space to process without feeling pressured or dismissed.
No matter how long you’ve been in infusion—two months or twenty years—these moments are inevitable. The difference between a tense exchange and a productive conversation often comes down to having the right words ready before you need them. When you can respond with confidence, you strengthen trust, keep patients engaged in their own care, and ensure they leave the chair feeling respected, protected, and genuinely heard. The more we prepare for these moments, the more we can meet them with calm instead of scrambling for what to say. If you want to hear more stories, strategies, and real-world examples of how to navigate them, tune in to my conversation with Alicia Barron and Derek Fox on the INS Infusion Room podcast.
🎧 Listen here

About the author:
Kaitey Morgan, BSN, RN, CRNI, is the Chief Clinical Officer of the National Infusion Center Association (NICA). With extensive experience in infusion nursing, clinical education, and operational best practices, Kaitey leads NICA’s efforts to advance safe, accessible, and sustainable provider-administered therapies. She works closely with clinicians, infusion providers, and stakeholders to develop evidence-based clinical resources, education, and quality standards that support both patients and providers. Kaitey is passionate about improving infusion care delivery and ensuring patients have timely access to the treatments they need.