From the Broomstick of Julie Baak
Pharmacy Benefit Managers (PBM) are the middlemen that do none of the work and make most of the money.
Fun Fact: PBMs have their MBAs tell MDs which drugs (formulary) they can prescribe based on how much money the PBM can make instead of clinical efficiency and the welfare of the patient(s). These ‘formularies’ are created based on drug manufacturers paying bribes and kickbacks in the forms of rebates, fees, and/or discounts in exchange for inclusion on this formulary list.
(Need a refresher on PBM Transparency? Click here. )
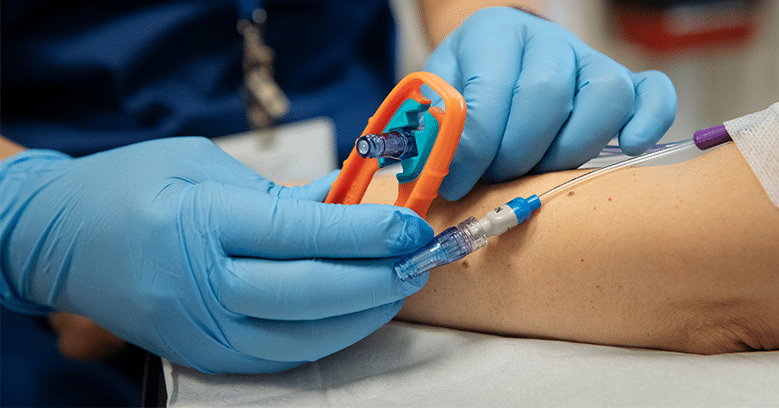
PBMs also get to ‘take back’ even more money (also known as ‘claw backs’) from independent pharmacies in Direct and Indirect Remuneration (DIR fees) and saddle independent physician infusion centers with admin burdens that require more staff.
Fun Fact Example: Think of a fox ‘guarding’ a hen house and you now understand the 3 PBMs (OptumRX, CVS and Express Scripts).
In a Pew Research study from March 2019, drug manufactures paid PBMs $10.2 Billion in rebates, fees, kickbacks, and/or bribes in 2012. (Yep – that is Billion with a ‘B’.) Then 4 years later in 2016, the drug manufactures paid PBMs $22.4 Billion. (Yep – Billions with another ‘B’.) Wow! If you are wondering, ‘How do I get in on this?’, well, you can’t. Not so surprisingly, the PBMs did NOT share these fees with their health-plan clients (the employers). Let’s give a ‘shout out’ to AT&T, UPS, Boeing, and Mallinkrodt, as your employees are paying for the yachts of the PBMs leadership instead of providing value to your working folks. That friends, is what no regulation looks like. Profits on the backs of the patients, employers, physicians, pharmacists and of course, the taxpayer.
This little perverse, predatory incentive is in the PBMs best interest to give preferential, formulary status to the highest priced drugs because the more expensive the drug is, the more money the PBM makes. For example, that is why Rheumatoid Arthritis patients must first try and fail Humira ($35k annual spend) AND Enbrel ($36k annual spend) BEFORE the PBMs ‘allow’ the physician to prescribe Simponi Aria infusions ($18k annual spend). Go ahead, check my math, the proof is in the proverbial pudding by seeing the outlandish profits posted year after year from OptumRX, CVS Specialty Pharmacy and Express Scripts.
What can your practice do? Advocate. It’s a mindset. It’s a game. You can learn and master this.
Be sure to sign up for NICA Advocacy updates to stay in the know about current and future PBM legislation.
Julie Baak is the Practice Manager of the Arthritis Center in Bridgeton, Missouri. Her NICA blog is called “From the Broomstick of Julie Baak”. Have comments, topic requests, or question for Julie? Please comment down below!