By: Kay Coulter, RN, CRNI, VA-BC
In the insurance industry there’s a saying about how you don’t know you’re facing litigation until it’s too late. Ambulatory Infusion Center providers can tell you risk management is key to protecting patients from harm and staff from lawsuits. IV Therapy Practice Pearls will offer current evidence-based principles, practice points and information related to the placement of peripheral vascular access devices, as well as the delivery of IV fluids and medications. Additionally, it will provide “tips & tricks” for the successful insertion of a peripheral IV catheter.
Our first topic will be Legal Issues Related to IV Therapy. Negligence is an important legal term that every clinician who practices IV therapy would know in order to avoid liability. The Infusion Nurses Society publishes Infusion Therapy Standards of Practice. These standards provide current, evidence-based information and practice statements for vascular access and the delivery of infusates to patients. One of these standards, often unknown, relates to the number of times a single clinician may attempt to accomplish IV access.
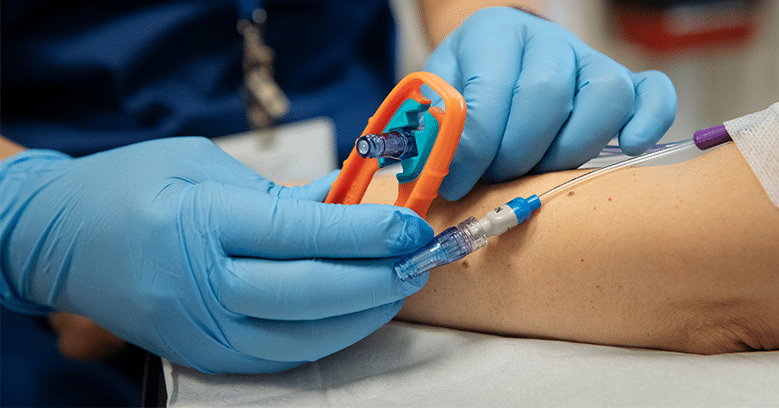
Standard #34: Vascular Access Device Placement (Point G) states “Restrict PIVC insertion attempts to no more than 2 (two) attempts per clinician at PIVC insertion. Multiple unsuccessful attempts cause pain to the patient, delay treatment, limit future vascular access, increase cost, and increase the risk for complications.” (#1) “After 2 (two) unsuccessful attempts, escalate to a clinician with a higher skill level and/or consider alternative routes of medication administration.” A clinician who attempts to place a peripheral IV more than two times violates INS Standards of Practice and could actually be accused of negligence.
Inappropriate site selection for the placement of a peripheral IV catheter can also result in a claim of negligence against the clinician. Placement of an IV catheter into the cephalic vein at the wrist flexion area or inner wrist could lead to nerve injury.
INS Standard #48: Nerve Injury (Point B) states “Recognize that some common sites have a greater risk of nerve injury; however, selecting specific peripheral venous and arterial puncture sites for the purpose of avoiding nerves is not always possible. As nerves cross a joint of the upper or lower extremity, there is an increase in neural tissue, increasing the risk of nerve injury in these areas. Motor, sensory, and/or autonomic nerve injury are possible due to direct nerve puncture or nerve compression. (1) Use caution with the following venous sites due to increased risk of nerve damage: (a) Cephalic vein at the radial wrist with potential injury to the superficial radial nerve. (b) Volar (inner) aspect of the wrist with potential injury to the median nerve.”
The INS Infusion Therapy Standards of Practice are evidence-based and are routinely used as a legal tool in medical malpractice cases. All policy and procedures related to the practice of IV therapy would be written according to these standards and published references. Two leading IV therapy reference books are the Infusion Nurses Society Infusion Nursing An Evidence-Based Approach and Phillips’s Manual of IV Therapeutics by Lisa Gorski. IV therapy practice that complies with current, evidence-based IV therapy textbooks and the INS Infusion Therapy Standards of Practice will keep patients safe and help to avoid liability for the clinician, as well as the organization.
Tips & Tricks for Peripheral IV Catheter Insertion
Apply a tourniquet taut enough to diminish venous return to the heart and still allow for arterial flow! A tourniquet that is applied too tight will actually restrict arterial blood flow and the veins will not receive sufficient blood flow to distend available veins. When a tourniquet is applied with a “vengeance” the clinician ultimately gets in their own way and reduces the chance of a successful IV catheter insertion.
About the Author
Kay Coulter, RN, CRNI, VA-BC Owner, Principal Instructor & Legal Nurse Consultant, Infusion Knowledge, Inc, is a nationally recognized infusion therapy clinician who has over 35 years of experience related to the specialty practice of infusion therapy. She has dedicated numerous years providing I.V. therapy-related education and consulting to all levels of healthcare providers, institutions, and organizations. Kay is the Co-founder, Executive Director and Principal Instructor for Infusion Knowledge, Inc. where she presents on all aspects of I.V. Therapy Education, Infusion-Related Legal Issues and PICC Qualification. She personally created the well-known CRNI® Review Program, which has been assisting nurses to successfully pass the CRNI® Exam for over 20 years; and most recently the VA-BC™ Exam Review Program. Kay is qualified as a Legal Nurse Consultant and has been retained as an expert witness for clinical infusion therapy legal matters.
About the National Infusion Center Association
NICA is dedicated to ensuring that the nation’s infusion centers remain a safe, more efficient, and more cost-effective alternative to hospital settings for consistent, high-quality care.
Infusion providers have a vested interest in the sustainability of the infusion delivery channel and its ability to serve vulnerable patient populations. NICA Provider Members have a voice and a seat at the table to inform NICA’s activities and the opportunity to remain highly engaged in the expansion and optimization of the infusion industry. Learn more about becoming a NICA member, here: https://infusioncenter.org/member-partner-page
Is your organization interested in becoming a featured subject matter expert on The Infusion Blog? Email [email protected] to inquire about opportunities for participation.