Written by Angie Baker and Stef Parks, Leaders in Patient Access and Reimbursement
As many drug manufacturers continue to develop new and innovative therapies for multiple disease states, we continue to see an evolution in the system through which payers (insurance companies/PBMs) use to process and pay claims. Copay accumulators have been present in the specialty pharmacy space for oral drugs for some time, causing many challenges for chronically ill patients as they fall under financial hardship. This hardship can increase the likelihood of treatment non-adherence, and can ultimately lead to advanced disease state. Additionally, patients who continue treatment may incur significant debt for long term costly treatments.
Pharmaceutical manufacturers offer copayment offset/assistance programs (also called copay cards or coupons) that cover the beneficiary’s out-of-pocket costs for a brand-name drug. These programs support beneficiaries with commercial insurance, but they cannot be used by enrollees in government programs such as Medicare Part D.
Copay Accumulator
A copay accumulator – or accumulator adjustment program – is a strategy used by insurance companies and Pharmacy Benefit Managers (PBMs) that stop manufacturer copay assistance coupons from counting towards two costs: 1) the deductible and 2) the maximum out-of-pocket spending.
As drug manufacturers attempt to create programs to subsidize out-of-pocket cost for patients, the payers reduce the value of these programs by exhausting such funds while also requiring the patients to pay their deductibles and coinsurance up to their out-of-pockets to obtain their medications. Does this mean the payer/ pharmacy benefit manager (PBM) is double-dipping?
Below is an example of a historical payment model for medication versus an accumulator model. For this example, the patient has a $2,000 deductible, 20% coinsurance, and a $4,000 out of pocket max. The drug in this example is $2,000 per month:
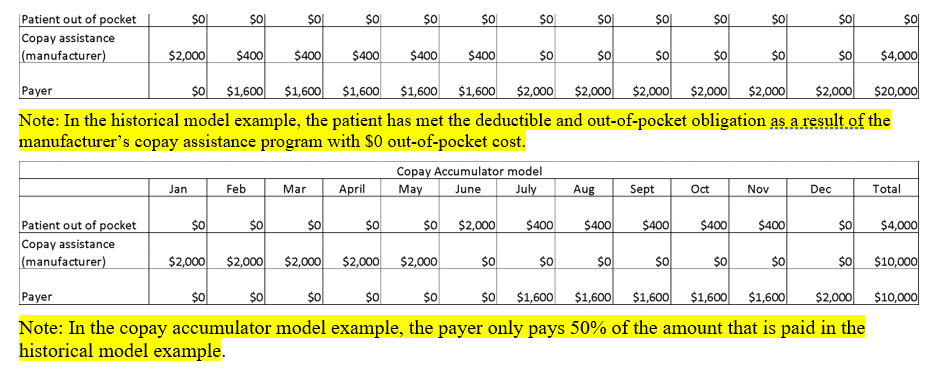
The difference in the copay accumulator model is the increase in the manufacturer’s contribution and the decrease in the payer’s expense. In addition to the increase in the manufacturer’s subsidy, the patient’s total out-of-pocket cost based on this example increases from $0 annually to $4,000 in order to satisfy the deductible, coinsurance, and out-of-pocket of the plan.
It’s evident after reviewing the example above that the only real benefactors of the copay accumulator model are the payers. As a result, the patients, who are the customers of the payers, suffer financially.
Copay maximizers, while similar, are a bit different.
Copay Maximizer
Under a copay maximizer, the full value of the manufacturer’s copayment program is applied evenly throughout the benefit year. A maximizer has an advantage over an accumulator because it reduces or eliminates the patient’s out-of-pocket obligations.
For example: When a patient is enrolled in a maximizer plan, the plan will take into consideration the pharmaceutical manufacturer’s monthly coupon value and slightly increase the copayment amount due each month, resulting in patient out-of-pocket cost, deductible contribution, and out-of-pocket max.
Best Practices for Providers to Address Copay Accumulators
- Investigate patient’s plan thoroughly during the benefit investigation process to identify plans that include an accumulator adjustment program
- Anticipate and prepare for an increase of copay accumulator plans in 2021
- Provide education to patients when you identify they are enrolled in plans that includes an accumulator adjustment program
- Counsel patients on their benefits for the specialty drug and how their financial obligation can be impacted during their therapy journey
Take Note of the Following
- Copay Card Yearly Benefit
- Monthly Copay Cost
- Identify which month the patient will exceed the copay card benefit based on monthly copay cost and the yearly copay card benefit max
- Educate the patient and provide resources to access manufacturer patient assistance programs
- If there is a financial hardship and the patient cannot afford the monthly copay cost of specialty medication, advise the patient to contact the patient assistance program a month prior to exceeding the copay card benefit to ensure timely enrollment and avoid a delay in therapy
Now is the time to act! As we are within the open enrollment period, it is a great time to investigate other plans if patients are affected by this challenge. Remind patients that they may have to dig deep into the fine print to determine if a specific health plan has a copay accumulator program. Remember to review the limitations and plan exclusions and ask how copay assistance funds from a manufacturer are applied and how they affect a patient’s out-of-pocket cost.