The following post is written by Sumaira Ahmed, matriarch of The Sumaira Foundation, a 501(c)(3) organization dedicated to generating global awareness of neuromyelitis optica spectrum disorder (NMOSD), fundraising to help find a cure, and creating a community of support for patients and their caregivers.
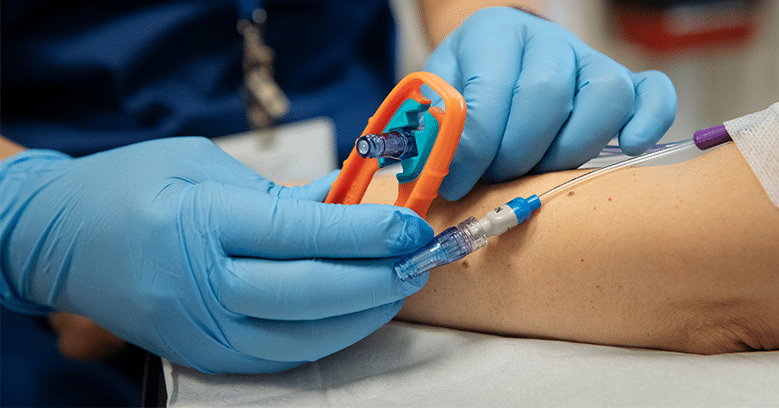
I used to be the kind of person who refused Tylenol because I didn’t like the idea of having medications floating around in my body. I had just turned 25 when I got diagnosed with neuromyelitis optica spectrum disorder and suddenly, I was taking 18 pills a day and receiving infusions. I won’t lie, it was a difficult transition.
I remember the days leading up to my first outpatient infusion. I was nervous and terrified. I still had several unanswered questions. All I knew prior to my experience was that infusions usually treated very serious and complex diseases and could come with a plethora of unpleasant side effects. At that age, potential side effects from my infusions that scared me the most were hair loss and vomiting. (I am emetophobic – aka, I have a phobia of throwing up.)
My parents drove in from New Jersey to be by my side during my first outpatient infusion; they were just as stressed as I was. My mom even brought her Quran to read and pray while she sat next to me as I was hooked up to the pole for 7 hours.
I remember after completing the infusion thinking, “That’s it?” My family and I were pleasantly surprised and relieved as we walked out of the infusion clinic where I’d return about 100 more times in the three years that followed.
It was at that moment when I realized that the anticipation of the infusion appointment was more stressful than the infusion itself. I researched the therapy that was being used to treat my illness and the accompanied side effects. I maintained a diary of any and all symptoms, whether they were related to my diagnosis or not. I began listening to my body to understand what she needed to be as well as she could be amidst treatment. I emailed my doctors whenever I didn’t feel well, no matter how minor or major it was. I became a self-advocate and promised myself that I would do my best to NEVER go into a situation as it relates to my health as unprepared as I was that first time.
As an advocate and a patient who has had over 500 infusions over a span of five years, I’ve got some advice to offer to my fellow infusion spoonies:
Shared Decision-Making | Many of us now have options for treatment. Shared decision-making is an important component of developing trust with your medical team and understanding your long-term treatment plan. Have a conversation with your care team. Ask questions. Understand the treatment plan. It is your body after all.
Do Your Homework | Talk to other patients who share the same diagnosis and are receiving the same infusions to understand what their experience has been like. Of course, every patient and experience is different but talking to others may help to answer some of your questions. Understand both short- and long-term side effects. This information can typically be found on the drug manufacturers websites.
Looking to connect with other patients who share your diagnosis? Sign up for free on the InfusionConfusion® Community forum and check out our patient rooms.
Stay Positive! | There’s no question that managing illness and receiving infusions can sometimes feel arduous, but a positive mind does go a LONG way! I used to say that I was “chained to the pole” during my infusions which led to all kinds of resentment and misery before, during, and after my treatments. Then, I changed the narrative and started referring to my infusions as “refuel sessions”, crediting the infusions for being one of the reasons I started to feel better.
Be Comfortable | Bring your most comfortable throw blanket. Read / listen to a book. Listen to music. Netflix & chill. FaceTime. Do whatever it takes to help you feel comfortable and be distracted while you refuel 😉